As states across the country debate whether to implement or update a fee schedule, the Workers Compensation Research Institute (WCRI) has released a new study that provides a tool to identify and better understand the implications of different types of fee regulations on hospital outpatient costs.
“Rising hospital costs have been a focus of recent policy debates in many states. To address this growth, WCRI has released the Hospital Outpatient Cost Index for Workers’ Compensation, 2nd Edition. This tool will help public policymakers and system stakeholders compare hospital outpatient costs across states, identify potential key cost drivers, and monitor the impact of reforms,” said Dr. Richard Victor, executive director of WCRI.
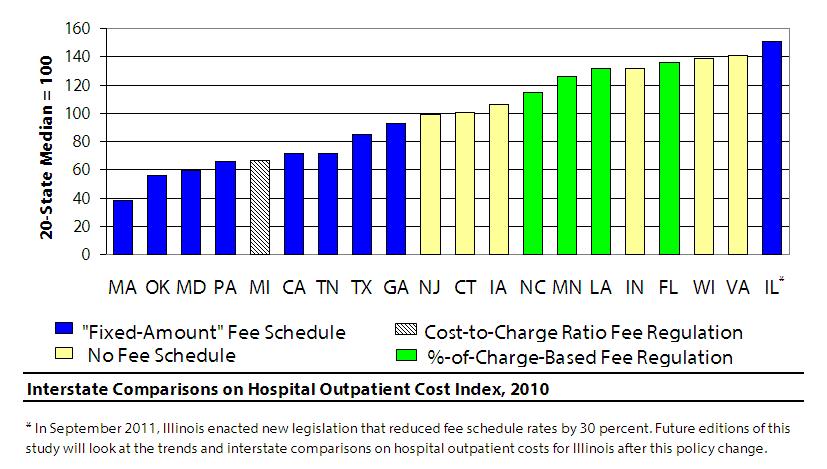
One of the most significant findings from the study was that states with hospital outpatient fee regulations based on a percent of charges had higher costs compared with states with “fixed-amount” fee schedules. “Fixed-amount” fee schedule refers to the type of regulation that assigns specific reimbursement amounts for each procedure or group of procedures. Four study states, Florida, Louisiana, Minnesota, and North Carolina, set their fee regulations for hospital outpatient services related to surgeries mainly based on percent of charges. The hospital outpatient costs in these states were 61 to 91 percent higher than the median of the study states with “fixed-amount” fee schedules.
This study also found states without fee schedules for hospital outpatient reimbursement had higher hospital costs for common surgeries compared to states with “fixed-amount” fee schedules. Six study states, Connecticut, Indiana, Iowa, New Jersey, Virginia, and Wisconsin, had no fee schedules as of 2010. The hospital outpatient costs in these states were 39 to 98 percent higher than the median of the study states with”fixed-amount” fee schedules.
The WCRI study found that states with “fixed-amount” fee schedules had relatively lower costs among the 20 study states. As of 2010, nine study states, California, Georgia, Illinois, Maryland, Massachusetts, Oklahoma, Pennsylvania, Tennessee, and Texas, had “fixed-amount” fee schedules for hospital outpatient services. The hospital outpatient costs in the median of these states was 45 percent lower than the median of the study states with fee regulations based on percent of charges, and 40 percent lower compared to the median of the study states with no fee schedules.
Illinois was an exception among states with the “fixed-amount” fee schedules. The hospital outpatient costs in that state were significantly higher than the other study states with the same type of regulation as of 2010. Illinois enacted a new legislation in September 2011, which reduced the fee schedule rates by 30 percent. Future editions of this study will look at results for Illinois after the policy change.
This study includes 20 large states that represent 65 percent of the workers’ compensation benefits paid in the U.S. and covers a six-year period from 2005 to 2010. The states included in this study are California, Connecticut, Florida, Georgia, Illinois, Indiana, Iowa, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, New Jersey, North Carolina, Oklahoma, Pennsylvania, Tennessee, Texas, Virginia, and Wisconsin.
For more information on this study or how to purchase it, click on the following link: http://www.wcrinet.org/result/hosp_cost_index_2_result.html.
Source: WCRI
Was this article valuable?
Here are more articles you may enjoy.

 Founder of Auto Parts Maker Charged With Fraud That Wiped Out Billions
Founder of Auto Parts Maker Charged With Fraud That Wiped Out Billions  LA County Told to Pause $4B in Abuse Payouts as DA Probes Fraud Claims
LA County Told to Pause $4B in Abuse Payouts as DA Probes Fraud Claims  Portugal Rolls Out $2.9 Billion Aid as Deadly Flooding Spreads
Portugal Rolls Out $2.9 Billion Aid as Deadly Flooding Spreads  UBS Top Executives to Appear at Senate Hearing on Credit Suisse Nazi Accounts
UBS Top Executives to Appear at Senate Hearing on Credit Suisse Nazi Accounts 