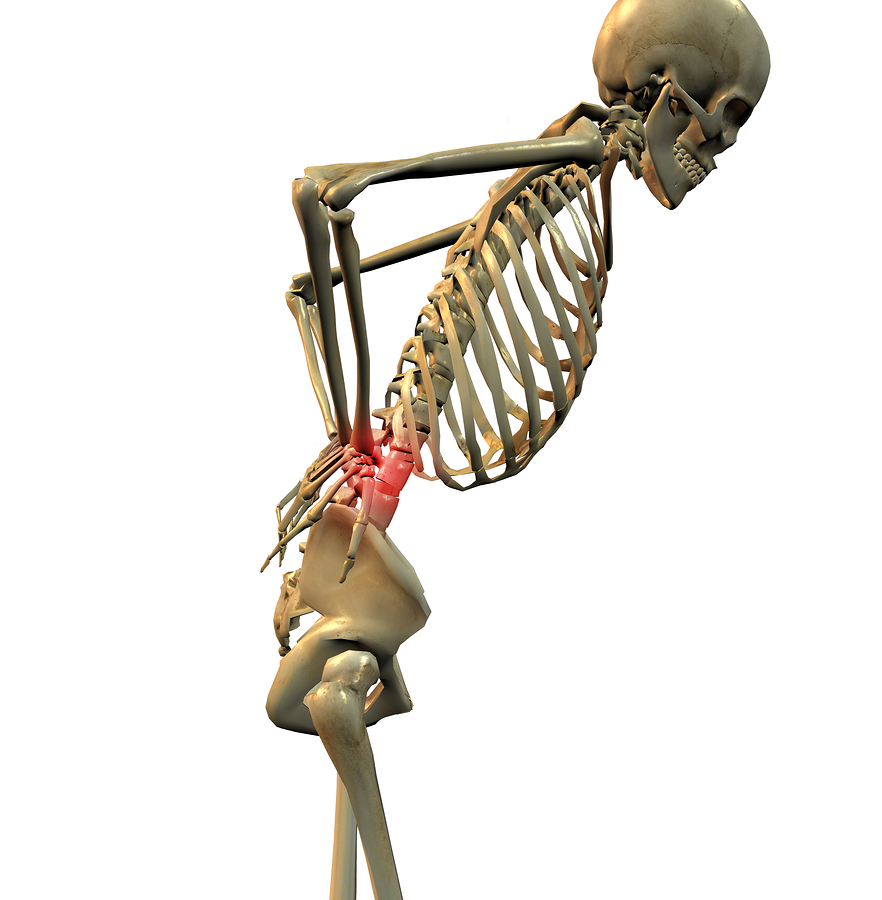
Inappropriate early use of Magnetic Resonance Imaging (MRI) to diagnose work-related lower back pain correlates with higher medical costs, unnecessary and ineffective procedures and prolonged disability, according to research conducted by the Liberty Mutual Research Institute for Safety.
 The most recent study published in Spine examined more than 3,000 workers compensation claims for disabling lower back pain over the course of a full year. Claims in which MRI was performed either within the first 30 days of pain onset or when there was no specific medical condition justifying the MRI yielded significantly higher medical costs, even after controlling for severity.
The most recent study published in Spine examined more than 3,000 workers compensation claims for disabling lower back pain over the course of a full year. Claims in which MRI was performed either within the first 30 days of pain onset or when there was no specific medical condition justifying the MRI yielded significantly higher medical costs, even after controlling for severity.
The study found these early or non-indicated MRIs led to a cascade of medical services in the six-month period post-MRI that included electromyography, nerve conduction testing, advanced imaging, injections or surgery. These procedures often occurred soon after the MRI and were 17 to nearly 55 times more likely to occur than in similar claims without MRI.
“Being a highly sensitive test, MRI will quite often reveal common age-related changes that have no correlation to the anatomical source of the lower back pain,” said Glenn S. Pransky, MD, MOccH, Center for Disability Research. “Leading evidence-based practice guidelines for lower back pain recommend against early MRI except for ‘red flag’ indications, such as severe trauma, infection or cancer. These guidelines suggest that, following a month trial of conservative treatment, MRI may then be considered if symptoms of sciatica/radiculopathy persist, but only to guide epidural steroid injections, or to provide more information if surgery is being considered. Because of a lack of evidence for improving care, the guidelines recommend that MRI is not indicated for non-radicular, non-specific back pain.”
Certain Tests and Treatments for Chronic Pain Should Be Questioned
Barbara S. Webster, lead author of the Research Institute’s studies said, “Adhering to guideline recommendations lessens this cascade effect of medical care where potentially unnecessary tests or procedures drive-up medical costs without evidence that they help to effectively treat the pain or shorten disability duration.”
In a prior study using a smaller sample of the same work-related lower back pain claims, early MRI recipients had far higher medical costs than non-MRI claims, averaging more than $12,000 higher. Early MRI recipients were also three times more likely to remain on disability than those who didn’t have MRI, even after controlling for a number of factors that influence these outcomes.
Handling Auto Bodily Injury Sore Back Claims
“The results of these studies provide additional evidence to promote shared decision-making conversations between providers and patients to help patients choose care that is supported by evidence and avoid tests and procedures that do not contribute to better outcomes,” Webster said.
The use of early imaging is one of many indicators for measuring appropriate clinical practices of Liberty Mutual’s network physicians and is used in the company’s Provider Performance Evaluation as part of its overall utilization review efforts to better ensure that injured workers are receiving high-quality and appropriate care.
“Clinical quality recommendations such as those developed by the National Committee for Quality Assurance and the American Board of Internal Medicine have emphasized for years that overuse of imaging does not represent good care for low back pain,” said Dr. William Gaines, associate national medical director, Liberty Mutual Commercial Insurance Claims. “These studies confirm that following best practices produces better outcomes for patients at lower costs.”
Source: Liberty Mutual Research Institute for Safety
Was this article valuable?
Here are more articles you may enjoy.

 LA County Told to Pause $4B in Abuse Payouts as DA Probes Fraud Claims
LA County Told to Pause $4B in Abuse Payouts as DA Probes Fraud Claims  US Will Test Infant Formula to See If Botulism Is Wider Risk
US Will Test Infant Formula to See If Botulism Is Wider Risk  Hackers Hit Sensitive Targets in 37 Nations in Spying Plot
Hackers Hit Sensitive Targets in 37 Nations in Spying Plot  Tesla Sued Over Crash That Trapped, Killed Massachusetts Driver
Tesla Sued Over Crash That Trapped, Killed Massachusetts Driver 