Medical science has moved forward by leaps and bounds in recent years, and yet for too many injured workers, their initial work-related injury and subsequent medical treatment is only the start of an all-too-familiar downward spiral that often ends in opioid addiction and permanent disability.
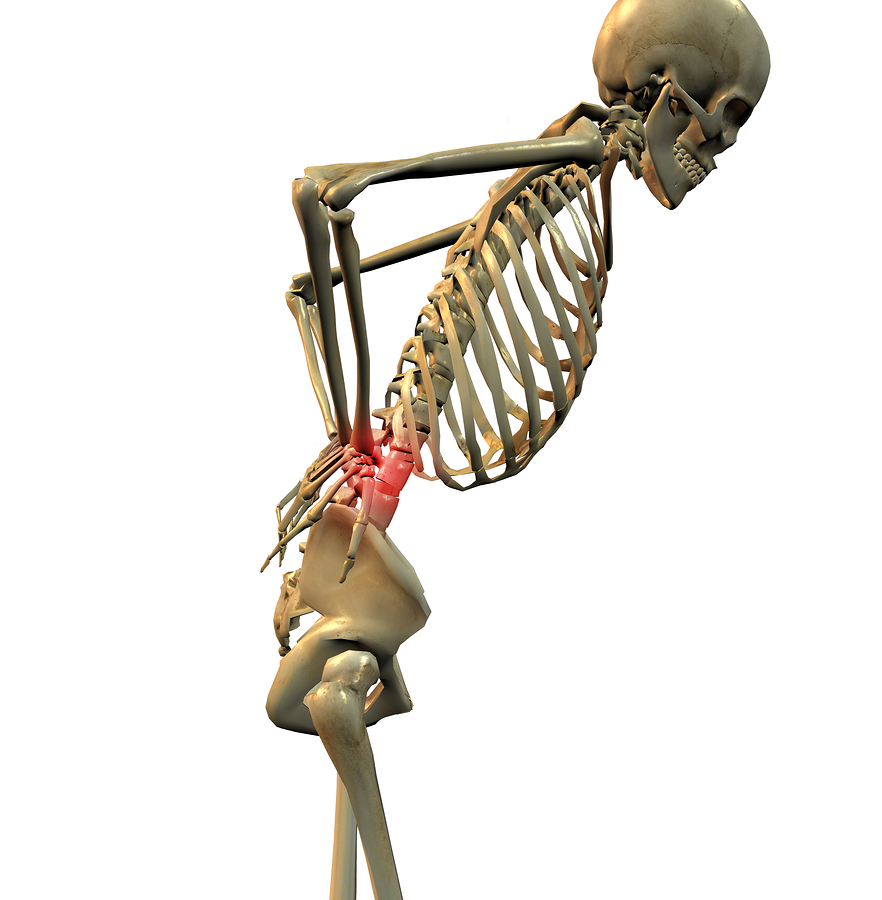
Even in cases without startling injuries, complaints of pain can lead to various conservative treatments including physical therapy, oral medications, creams and patches. If complaints of pain persist, different drugs or categories of drugs are tried, and if they fail, many injured workers will agree to surgical procedures. Surgery often not only fails to reduce the original complaints of pain, but can create entirely new scarring, adhesions, muscle and nerve injury, disuse, atrophy, and deconditioning. Sometimes a second or third surgery is attempted; often with a spiral of worsening outcomes. Sometimes more aggressive pain management procedures, such as the installation of spinal cord stimulators or continuous drug pumps are pursued. The outlook for recovery from disability is grim, and the chances of medical expenses ever being controlled vanish. Opioids are prescribed in increasing dosages due to the development of tolerance to the drugs. Yet the worker’s condition never improves. The worker is left not only in pain but also with disillusionment, depression, anxiety, and feelings of hopelessness.
At this point in the management of such a case, the comp carrier or employer writes the case off as hopeless, and funds an enormous Medicare Set-Aside and lump sum settlement.

What options are available to interrupt this predictable downward spiral? Studies have been underway now for a decade about the potential for using psychedelic therapies in controlled environments for the treatment of pain and depression.
These treatments raise the hairs on the back of my skeptical neck but are likely to become a big factor in workers’ comp pain treatments, one way or the other.
I have been practicing workers’ compensation defense litigation for more than thirty-five years. In that time, I have seen scores of hoaxes, frauds, and scams, and I have also seen the evolution of whole new classes of claims for conditions that transformed from highly disputed theories into generally accepted work-related disorders. I was at the front of the line of skeptics when “tight building syndrome” and “multiple chemical sensitivity” were in vogue and helped lead the campaign against unapproved, unproven, and remarkably expensive compounded pain creams. I fought against the notion that work-related cell phone use caused cancer, and challenged the theory that prostate cancer is caused by exposures experienced by firefighters. I am a card-carrying member of the workers’ compensation skeptic’s society.
As a defense lawyer and skeptic, I have always had a hard time finding empathy for workers claiming to have chronic pain, especially in the absence of objective data of a serious underlying disorder. Pain is easy to assert and hard to prove or disprove. Other than one-off challenges to the credibility of the claimant (surveillance evidence, record of inconsistent histories, or anatomical complaints unrelatable to physiology) there is no reliable way to assess whether someone is in pain that warrants treatment or justifies disability.
Not only is it difficult to determine if someone is in pain, and how much, it is difficult to tell what causes pain and what relieves it. The potential for large payouts of benefits and lump sum settlements is a strong factor that could lead a person to exaggerated complaints and encourage a claimant to fail at treatment. If a treatment were successful, case value would plummet.
It is widely suspected that the perception of pain can be the result of both physical and psychological influences. Some people become depressed due to pain and disability; some people who are depressed focus and magnify their pain and disability.
Treatments for pain have changed over time. Some, in retrospect, were fads, get-rich-quick schemes or flat-out frauds. Snake oil is a great example. It was peddled by charlatans as a cure for all sorts of problems including pain. Not only was there no evidence that the oil of any snake could cure pain, the con-artists selling these elixirs began selling snake oil potions that did not actually contain snake oil. Some contained innocuous ingredients like mineral oil – others contained poisons, cocaine or other addictive drugs. The combination of the skill of the salesman and the desperation of the person seeking relief resulted in huge sales. The problem was so rampant that snake oil concoctions were a major reason for the launch of the Food and Drug Administration – not because snake oil didn’t work – but because the potions being sold as snake oil did not contain real snake oil.
Treatments for pain and the often related condition of depression moved on from the foolish, like snake oil, to the intriguing, such as the use of hyperbaric chambers, to the purely hopeful, like eliminating wheat (or processed foods, or sugar, or dairy, etc.) from the diet. Many highly utilized pain treatments are still of unproven efficacy, such as chiropractic manipulation, acupuncture and magnetic therapies.
Big pharma is now at the heart of treatment for pain. Tried and true remedies from aspirin to acetaminophen work for many people. Drugs ranging from analgesics, muscle relaxants, and anti-convulsives to anti-depressants are commonly mixed and matched until there is a subjective report of pain relief. Dating back thousands of years, opium and other derived drugs were used for pain. By the 1970s, synthetic opioids became increasingly popular, and usages morphed from treating patients in the final days of cancer pain to virtually universal prescription after even modest surgical procedures. During the 2000s, opioid usage exploded and hundreds of thousands of people began dying from accidental or intentional opioid overdoses. Abuse and addiction became so widespread that pressure is mounting to reduce opioid prescription and usage, but opioids remain in the top five most frequently used drugs in workers’ compensation.
Costs in cases in which workers are on opioids have skyrocketed, not just due to the costs of the drugs, but also due to the fact that the drugs are incredibly addictive, and once started in the workers’ compensation arena, where utilization challenges often fail, they are likely to continue until the worker’s death. The drugs have side effects that require additional drugs and treatments, routine testing, and continuous monitoring, adding to expense and increasing settlement values.
An alternative under investigation is treatment with psychedelic drugs.
Psychedelics conjure up memories of LSD, college, magic mushrooms, peyote, and Timothy Leary. They were drugs that I recall being used by addicts, thrill-seekers, spiritual searchers and counter-culture hippies. But then again, I could say the same thing for marijuana, which is now a compensable drug under the comp laws of many states.
But one psychedelic drug seems to be leading the pack in general medical acceptance – ketamine. Psychedelic therapy with ketamine is now being used to treat depression. The first completely new anti-depressant drug created in the last 30 years is Spravato, which delivers a dose of ketamine via a nasal inhaler. This is a new concept – the FDA only began approving ketamine-based treatments for depression a couple of years ago.
Pain and depression often overlap, and the neuropathways in both conditions overlap. It is therefore not surprising that using ketamine for treatment of chronic pain has been attempted and will continue to gain in popularity. Near as I can tell, it is now legal to use ketamine as an off-label treatment for pain, with or without an overlapping diagnosis of depression.
Ketamine became a popular, quick acting anesthetic used during the Vietnam war. It has been used for surgical anesthesia and in veterinary medicine for decades. At certain doses, it can trigger hallucinations and other mind-altering status – hence its growing popularity as a street drug of abuse (“Special K”).
Ketamine should be familiar to most people in the workers’ compensation world. In the 1980s, people with RSD (now called CRPS) were often directed to special clinics overseas (because very few US institutions would consider administering such treatment) to be put into ketamine-induced comas. Upon recovery, some patients reported at least a temporary interruption in the intensity of their pain.
Ketamine showed up again in the 2010s, this time as an ingredient in topical compounded pain creams. There was little if any evidence that ketamine can be absorbed through the skin in a therapeutic amount, and even less evidence that it had a local impact when rubbed in, but due to the profit motivation of getting up to $12,000 per tube, pharmacies and doctors starting doling the stuff out like aspirin, until a wave of indictments, arrests, convictions, fraud suits and refusal to pay by key PBMs and carriers forced CPCs to the shelves of pharmaceutical history, right next to snake oil.
More recently, ketamine in sub-anesthetic doses is being used for conditions ranging from chronic migraines to fibromyalgia. Studies of the efficacy and safety of using ketamine to treat chronic pain are ongoing and results so far seem to be mixed to positive. There is a great upside potential for patients and for the world if ketamine turns out to be less addictive, less lethal, and less subject to abuse than opioids, especially if pain reduction is equal or better.
Ketamine, once typically delivered via IV infusion in a hospital setting, is now available in nasal spray, lozenge, and pill form. It is still a Schedule III controlled substance but is being used already by psychiatrists and therapists for treatment of depression, in conjunction with other therapies and under close supervision, and is making some headlines for efficacy.
Some studies report that ketamine, administered under close supervision in a clinical setting, can have a nearly immediate effect, and at least for depression, the effects can last up to 12 weeks until the next treatment. Reports on extent and duration of pain relief are more variable and less voluminous.
Since ketamine is an FDA approved drug, and some patients report it to be effective in reducing pain/depression, I have no doubt that in states that do not require use of drugs on a formulary and in states that do not allow the employer to control medical treatment, we will see a surge in ketoimine therapy. If the trend accelerates, it will be added to formularies and judges and Boards will start to require carriers to pay for the treatments. Ketamine treatments, at least for depression, are already approved by most major health insurance carriers. I don’t think that there would be a reasonable basis for a workers’ compensation carrier to deny ketamine treatment for depression, and if it overlaps, as it often does, with pain, carriers will also be under heavy pressure to approve these treatments.
Is this a good thing or a bad thing? If the treatments are proven to be effective in reducing pain, reducing or eliminating reliance on opioids, decreasing duration or percentage of disability or impairment, and decreasing the demand for surgery and post-surgical medical intervention to fix what the surgery itself caused, this could be a very good thing. If profit seekers artificially inflate the demand for the treatments, administer them without careful preparation, patient selection and follow up, or if further studies do not confirm efficacy, this could be another expensive and passing medical fad.
Was this article valuable?
Here are more articles you may enjoy.

 These Five Technologies Increase The Risk of Cyber Claims
These Five Technologies Increase The Risk of Cyber Claims  Canceled FEMA Review Council Vote Leaves Flood Insurance Reforms in Limbo
Canceled FEMA Review Council Vote Leaves Flood Insurance Reforms in Limbo  US Will Test Infant Formula to See If Botulism Is Wider Risk
US Will Test Infant Formula to See If Botulism Is Wider Risk  Charges Dropped Against ‘Poster Boy’ Contractor Accused of Insurance Fraud
Charges Dropped Against ‘Poster Boy’ Contractor Accused of Insurance Fraud 