Researchers say they have found a way to capture images of injuries from whiplash, a condition often associated with motor-vehicle accidents that is difficult to diagnose and treat.
An international team led by Harvard Medical School’s Department of Physical Medicine and Rehabilitation at Spaulding Rehabilitation Hospital in Boston said the new approach to scanning allows clinicians to better target medical treatments.
“An objective visualization and quantification of the injury and possible inflammation in whiplash-associated disorders would support a better diagnosis, strengthen patients’ subjective report of pain, and assist clinical decisions,” said the lead author, Clas Linnman, an assistant professor of physical medicine and rehabilitation at the Spaulding Neuroimaging Lab, according to an article posted online by Harvard Medical School.
Linnman said it has been difficult to detect and diagnose lesions related to the pain experienced by people with whiplash and there is no accepted concept for what causes the symptoms in whiplash-related disorders.
There were 4 million rear collisions in the US with 3 million whiplash injuries that cost $8 billion annually, according to 2016 paper by the Insurance Institute for Highway Safety. The IIHS said rear automatic braking is associated with the largest reduction in insurance claims and backing crashes reported to the police of any type of rear crash prevention system.
Until now, there have been few objective measurements available to confirm the existence of whiplash injuries.
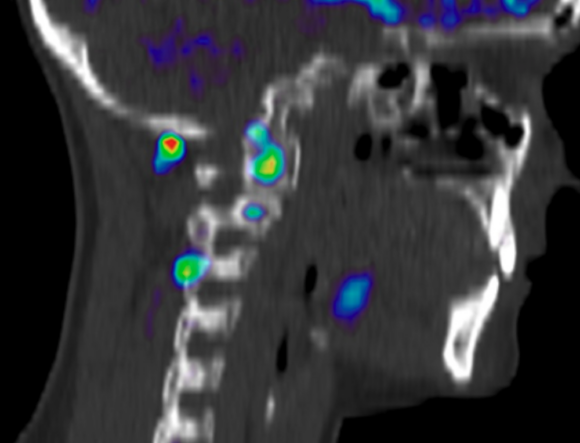
The study found that the molecular aspects of inflammation and possible tissue injuries in muscles and facet joints after an acute whiplash injury can be visualized, objectively quantified and followed over time by using positron emission tomography and computed tomography after an injection of D-deprenyl. The new approach to scanning “finally allows whiplash injuries to be visible,” Linnman said on Twitter.
The researchers from Harvard and Uppsala University in Sweden observed 16 adult patients who were admitted to Swedish emergency rooms after suffering whiplash injuries during car crashes. After D-deprenyl was administered intravenously, physicians conducted PET/CT scans of the neck region.
The scans revealed increased uptake of D-deprenyl in muscles, bones and joint tissue in patients’ upper neck region. In contrast, a conventional CT scan of the neck did not reveal any pathological findings, according to the study.
The patients were scanned again six months after injury. Those scans showed significantly improved neck disability ratings, cervical range of motion and pain levels correlated with fewer regions with elevated uptake of D-deprenyl.
“Nonetheless, the patients still experienced pain, disability and reduced range of motion, and elevated D-deprenyl uptake was still evident,” the study says. “This suggests that healing was progressing, but still ongoing at six-month follow-up in most patients, and that D-deprenyl PET holds potential to capture the process.”
The study was published in the July 2 edition of Pain, a journal published by the International Association for the Study of Pain.
Was this article valuable?
Here are more articles you may enjoy.

 Hackers Hit Sensitive Targets in 37 Nations in Spying Plot
Hackers Hit Sensitive Targets in 37 Nations in Spying Plot  Elon Musk Alone Can’t Explain Tesla’s Owner Exodus
Elon Musk Alone Can’t Explain Tesla’s Owner Exodus  Credit Suisse Nazi Probe Reveals Fresh SS Ties, Senator Says
Credit Suisse Nazi Probe Reveals Fresh SS Ties, Senator Says  One out of 10 Cars Sold in Europe Is Now Made by a Chinese Brand
One out of 10 Cars Sold in Europe Is Now Made by a Chinese Brand 