A study on the use of spinal fusion surgeries in California workers’ compensation shows that in 60 percent of spinal fusion claims the initial report of injury was for a sprain or strain, a majority of the fusions occurred within two years of the injury, and as the claims aged more than 20 percent involved at least one subsequent fusion surgery.
The analysis by the California Workers’ Compensation Institute is based on data from more than 18,266 California work injury claims from accident years 2000 through 2014 in which one or more spinal fusions were performed.
The CWCI identified spinal fusion claim characteristics (cause and nature of injury, part of the spine that was fused and the number of spinal segments involved), patient demographics, the presence of comorbidities and the average amounts paid in indemnity and medical benefits.
The study also measured the timing of the initial fusion and the presence and timing of any subsequent fusions, independent medical review outcomes for spinal fusion requests, utilization trends for MRIs, pre- and post-surgery physical therapy and the level of pre- and post-surgical opioid use.
The findings:
- Men accounted for more than 64 percent of the spinal fusion claims in each of the 15 years studied, and average amounts paid across the entire span were higher for males than females (15.5 percent more for temporary disability, 27.1 percent more for permanent disability and 16 percent more for medical).
- 62 percent of the claims that involved a spinal fusion were initially reported as strain and sprains; followed by cumulative traumas (including mental stress), which comprised 14 percent.
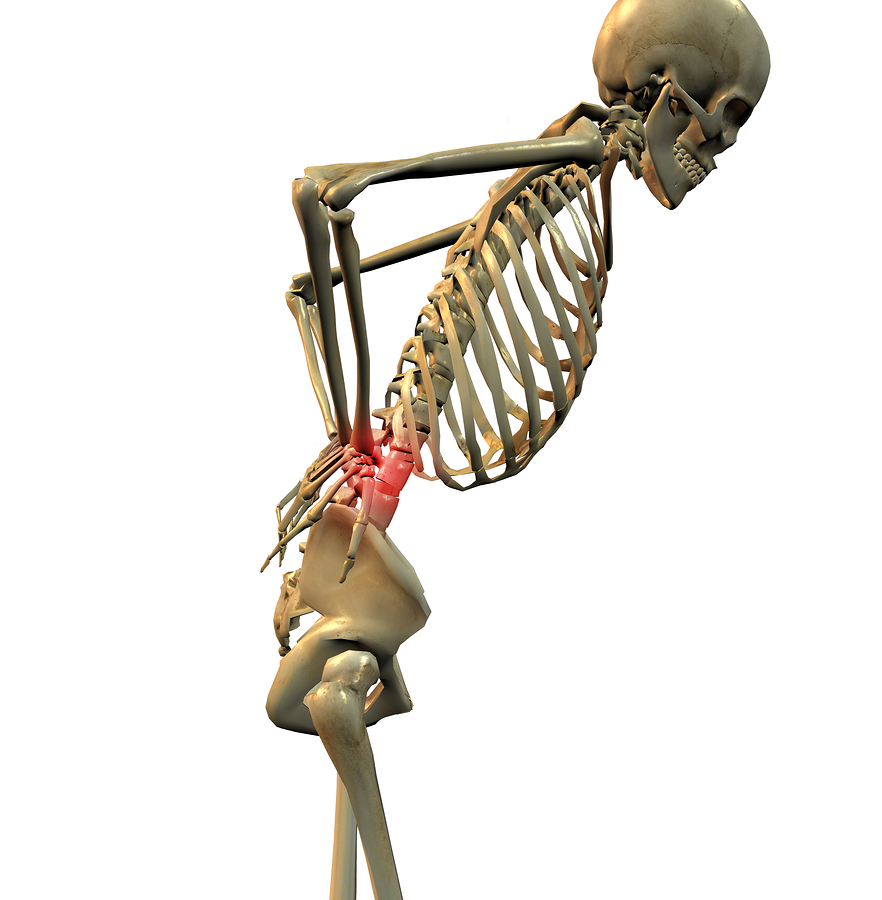
- Lumbar fusions accounted for nearly half of the workers’ comp spinal fusions, while fusions involving additional vertebral segments represented one-third of all fusions.
- Mental health disorders were the leading comorbidity (noted in 37 percent of spinal fusion cases), while 29.9 percent involved circulatory problems and 17.1 percent listed substance abuse as a comorbid condition.
- Loss payments on medical back diagnoses without spinal cord involvement averaged as much as $378,392 in AY 2003, or 6.7 times the average for similar claims without a spinal fusion.
Was this article valuable?
Here are more articles you may enjoy.

 UBS Top Executives to Appear at Senate Hearing on Credit Suisse Nazi Accounts
UBS Top Executives to Appear at Senate Hearing on Credit Suisse Nazi Accounts  These Five Technologies Increase The Risk of Cyber Claims
These Five Technologies Increase The Risk of Cyber Claims  US Will Test Infant Formula to See If Botulism Is Wider Risk
US Will Test Infant Formula to See If Botulism Is Wider Risk  LA County Told to Pause $4B in Abuse Payouts as DA Probes Fraud Claims
LA County Told to Pause $4B in Abuse Payouts as DA Probes Fraud Claims 